Is Aging A Disease?

Getting a drug approved for aging is a major challenge because regulatory bodies in the US and Europe have not, until very recently, recognized “aging” as a medical condition that needs treating. Aging has been considered just a natural part of adult life, not a disease. As a result, drug companies have invested very little research dollars into aging because there was no "disease" to cure, and no way to patent any drugs. Most of the researc h has come from anti-aging organizations such as the National Institute on Aging.
Inflammation is one of the mechanisms behind aging, so aspirin and statins could be effective drugs in part because they slow aging, says Brian Kennedy, who heads the Buck Institute for Research on Aging in Novato, California. “Part of why aspirin and statins are such effective heart drugs is because they are slowing aging”, says Kennedy.
The fact that common mechanisms seem to be behind the major diseases of aging, like heart disease, stroke and dementia, is good news as it suggests we should be able to extend our lifespan while also extending healthspan.
“Aging is by far the best predictor of whether people will develop a chronic disease like heart disease, stroke, cancer, dementia or osteoarthritis,” Dr. James. Kirkland, director of the Kogod Center for Aging at the Mayo Clinic, said in an interview. “Aging way outstrips all other risk factors.”
While some existing medicines have the potential to extend our lifespan by a few years, drug companies want to develop more potent longevity agents that can be "patented". One of the answers is for drug firms to initially seek approval of their drugs as a treatment for a specific age-related condition, such as heart disease or diabetes. Then, seek to demonstrate their broader powers with a "patented" drug. Top
Vitamin NR Extends Health And Life
NAD is the term used to describe a cellular metabolite (small cell molecule) called nicotinamide adenine dinucleotide (or simply NAD). NAD is found in every cell in the body and is essential to life. NAD enables the transfer of energy from the foods we eat to vital cell functions. It is also required to “turn off” genes that accelerate degenerative aging processes.
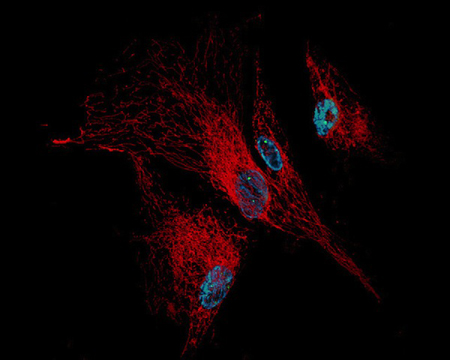
As NAD levels decline, the mitochondrial function (energy production of our cells) is impaired, resulting in fewer mitochondria surviving. This vicious cycle of mitochondrial depletion results in many of the physical symptoms of aging. In the picture to the left are human cells showing their mitochondria networks (red), their nuclear DNA (blue) and a few sites of DNA damage (small green dots). Research shows that NAD has a unique ability to protect tissues, induce DNA repair, and increase life span.
A vitamin called nicotinamide riboside (NR) has been found to increase NAD levels and in the process provide an extraordinary range of longevity benefits that promises to change how we combat aging. Directly boosting NAD with NR presents an effective strategy for preventing the natural decline in cellular energy as we age. The roundworm, C. Elegans, was made to survive as much as 16% longer when supplemented with NR. Its life span extension was demonstrated to result from a roughly 50% increase in healthy mitochondrial oxygen consumption, a measure of mitochondrial efficiency. NR is a non-prescription drug and can be purchased from LifeExtension here.
In the first controlled clinical trial of NR for humans, researchers have shown that the compound is safe for humans and increases levels of NAD that is critical for cellular energy production and protection against stress and DNA damage. The new research, reported in October, 2016 in the journal Nature Communications, was led by Charles Brenner, PhD pictured to the left.
The human trial involved six men and six women, all healthy. Each participant received single oral doses of 100 mg, 300 mg, or 1,000 mg of NR in a different sequence with a seven-day gap between doses. After each dose, blood and urine samples were collected and analyzed by Brenner’s lab to measure various NAD metabolites. The trial showed that the NR vitamin increased NAD metabolism by amounts directly related to the dose, and there were no serious side effects with any of the doses.
Prior to the formal clinical trial, Charles Brenner conducted a pilot human study on himself. In 2004, he had discovered that NR is a natural product found in milk and that there is a pathway to convert NR to NAD in people. More than a decade of research on NR metabolic pathways and health effects in mice and rats had convinced him that NR supplementation had a real promise to improve human health and wellness. In 2014, he conducted an experiment in which he took 1 gram of NR once a day for seven days, and his team analyzed blood and urine samples using mass spectrometry. The experiment showed that Brenner’s blood NAD increased by about 2.7 times. In addition, he did not experience any negative side effects taking NR. Top
Booster NMN Potentially Reverses Aging and Helps NASA
In a study at Harvard and the University of New South Wales (UNSW) in Australia, researchers discovered a revolutionary drug that reverses aging, improves DNA repair and could even help NASA get its astronauts to Mars. Treating mice with an NAD booster, called NMN, improved their cells' ability to repair DNA damage caused by radiation exposure and/or old age. "The cells of the old mice were indistinguishable from the young mice after just one week of treatment," said lead author Professor David Sinclair of the Harvard Medical School (HMS) and UNSW School of Medical Sciences, pictured to the left.
This work has excited NASA, which is dealing with the challenge of keeping its astronauts healthy during a four-year mission to Mars. Even on short missions, astronauts experience accelerated aging from cosmic radiation, suffering from muscle weakness, memory loss and other symptoms when they return. On a trip to Mars, the situation would be far worse. Five per cent of the astronauts' cells would die and their chances of cancer would approach 100 per cent.
DNA repair is essential for cell vitality, cell survival, and cancer prevention, yet the cells’ ability to patch up damaged DNA declines with age for reasons not fully understood. Now, research at HMS and UNSW reveals a critical step in a molecular chain of events that allows cells to mend their broken DNA.
NAD, identified a century ago, is already known for its role as a controller of cell-damaging oxidation. The mice experiments showed that NMN mitigates age-related DNA damage and wards off DNA damage from radiation exposure. The researchers found that when NAD is plentiful, it prevents protein DBC1 from binding to protein PARP1. The combination of the two proteins (DBC1 and PARP1) who like each other and closely bind together whenever they can, causes damaged DNA not to mend.

As NAD declines with age, fewer and fewer NAD molecules are around to stop the harmful interaction between DBC1 and PARP1. The result: DNA breaks go unrepaired and, as these breaks accumulate over time, they precipitate cell damage, cell death, and the eventual loss of an organ's function. To determine how the proteins interact beyond the lab dish and in living organisms, the researchers treated young and old mice with the NAD precursor NMN, which makes up half of an NAD molecule. (In chemistry a precursor is a compound that participates in a chemical reaction that produces another compound.) NAD is too large to cross the cell membrane, but NMN can slip across it easily. Once inside the cell, NMN binds to another NMN molecule to form new NAD.
After receiving NMN in their drinking water for a week, the old mice showed marked differences in NAD levels. NAD levels in the livers of old mice shot up to levels similar to those seen in younger mice. The cells of mice treated with NMN showed fewer PARP1 and DBC1 molecules binding together. In a final step, scientists exposed mice to DNA damaging radiation. Cells of animals pre-treated with NMN showed lower levels of DNA damage. However, the protective effect was seen even in mice treated with NMN after radiation exposure. Great stuff! Human trials of NMN therapy are planned to begin within six months. Stay tuned... Top
Diabetes Drug Increases Human Lifespan
Metformin is the most popular prescription diabetes drug in the world, with over 60 million prescriptions filled in the US alone each year. During 2014, a UK study of 78,000 diabetes patients being treated with Metformin not only lived longer than other diabetic patients, but also lived 15% longer than the healthy control sample of 90,000 people. 15% longer is about 12 years or a nice age of about 92 years.
In 2015 Cardiff University in the UK found that when patients with diabetes were given the drug Metformin they in fact lived longer than others without the condition, even though they should have died eight years earlier on average. Lets settle for a 10 year increase as the average of the two studies.
When Belgian researchers tested Metformin on tiny roundworms, the worms not only aged slower, but they also stayed healthier longer. They did not slow down or develop wrinkles. Mice treated with Metformin increased their lifespan by nearly 40 per cent and their bones were also stronger.
Up until very recently, the US Food and Drug Administration viewed aging as a natural process that could not be stopped. However, the FDA has allowed a US aging trial to start in the fourth quarter of 2016 with its blessing. The clinical trial is called Targeting Aging with Metformin (TAME) and it is formally investigating whether the drug is capable of slowing and/or stopping degenerative human diseases and heart conditions. Scientists plan to recruit 3,000 people in their 70s and 80s who either have or are at risk of having major diseases. The trial is expected to take five to seven years.
During our lifetime, billions of cell divisions must occur to keep our bodies functioning correctly. As we age and cell problems grow, the body can no longer quickly repair damage. In the case of cancer, cells no longer have the ability to get rid of mutations and tumors grow wildly. In Alzheimer’s the brain stops clearing out sticky plaques and dementia develops. The reason Metformin delays the aging process is because "it increases the number of oxygen molecules released into every cell" which is thought to boost robustness and longevity. Everyone should take 2,000 mg of Metforman every day. Top
What Is Immunotherapy?
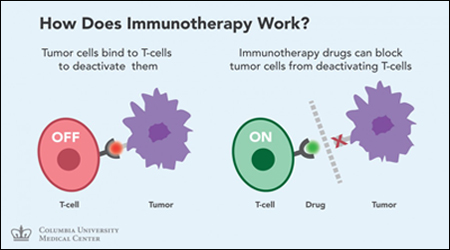
Immunotherapy is a treatment that uses parts of a person’s immune system to fight cancer. This can be done in a couple of ways:
- Stimulating your own immune system to work harder or smarter to attack cancer cells.
- Giving you immune system components, such as man-made immune system proteins.
In the last few decades immunotherapy has become an important part of treating some types of cancer. Newer types of immune treatments are now being studied, and they will impact how we treat cancer in the future. Immunotherapy includes treatments that work in different ways. Some boost the body’s immune system in a very general way. Others help train the immune system to attack certain cancer cells specifically. Immunotherapy works better for some types of cancer than for others. It is used by itself for some cancers, but for others it seems to work better when used in combination with other types of treatment.
How Does The Normal Immune System Work?
The immune system keeps track of all of the substances normally found in the body. Any new substance that the immune system does not recognize raises an alarm, causing the immune system to attack it. For example, germs contain substances such as certain proteins that are not normally found in the human body. The immune system sees these as “foreign” and attacks them. The immune response can destroy almost anything containing a foreign substance.
However, the immune system has a tougher time targeting cancer cells. This is because cancer starts when certain cells become altered and start to grow out of control. The immune system does not always recognize cancer cells as foreign because they start out as a bunch of normal cells. Cancer cells themselves can also give off substances that keep the immune system in check. To overcome this, researchers have found ways to help the immune system recognize cancer cells and strengthen its response so that it will destroy the cancer.
The main types of immunotherapy now being used to treat cancer include:
- Immune checkpoint inhibitors: These drugs basically take the ‘brakes’ off the immune system, which helps it recognize and attack cancer cells.
- Monoclonal antibodies: These are man-made versions of immune system proteins. Antibodies can be very useful in treating cancer because they can be designed to attack a very specific part of a cancer cell.
- Cancer vaccines: Vaccines are substances put into the body to start an immune response against certain diseases. We usually think of them as being given to healthy people to help prevent infections. But some vaccines can help prevent or treat cancer.
- Other non-specific immunotherapies: These treatments boost the immune system in a general way, but this can still help the immune system attack cancer cells.
Jim Allison Makes Immunotherapy A Cancer Breakthrough
Jim Allison is a basic scientist at the MD Anderson Cancer Center in Houston, Texas. He is a Ph. D. rather than an M.D. and works with cells and molecules rather than patients. However he is the Chairman of the Immunology Department and has made one of the most significant breakthroughs in cancer research in recent years. He has received many prestigious awards and many people think he will ultimately receive a Nobel Prize.
Back in the mid-90s, Allison and another research group discovered that a molecule called CTLA-4 acted as a brake on T-cells (powerful "killer cells" that are part of the human immune system) preventing them from wildly attacking the body's own cells.
See the picture of some T-Cells below. The CTLA-4 molecule functions as a "checkpoint" turning off the T-cells. Allison (all by himself) wondered if it could be used in cancer treatment.
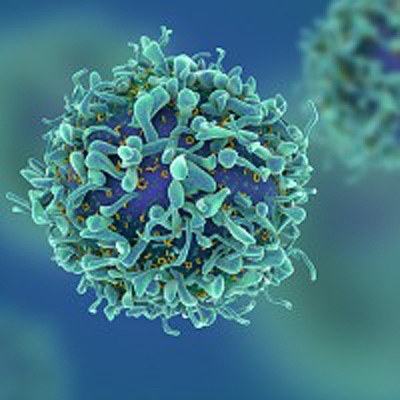
Allison's team created an antibody designed to block the CTLA-4 receptor. He began an experiment to see if blocking CTLA-4 would allow the immune system's T-cells to attack cancer tumors in mice. Not only did the mice tumors disappear, but the mice were now immune to future cancer attacks from the same type of cancer. At first he did not believe the results, so he repeated the experiment again, with the same results. Because the checkpoint inhibitor targeted T-cells instead of tumor cells, the cancer cells do not respond by mutating and developing resistance like they do with chemotherapy and other treatments.
After publishing his results in Science Magazine in 1996, Allison began looking for a pharmaceutical company to develop a CTLA-4 inhibitor for humans. But, Allison hit a wall. After two years of rejections, a small New Jersey based company called Medarex said yes.
It began working with Allison to develop a medication and by 2001, five years later, ipilimumab ("ipi" for short) was ready for testing. Early trials of the drug (just to see if it was safe) succeeded so greatly that Bristol Myers bought Medarex for $2.4 billion. The drug, now known as Yervoy, became the first "checkpoint inhibitor". Without the brakes, the immune system can recognize cancer as an enemy and destroy it.
Today, Allen continues to work on one of the problems with immunotherapy. Only 20% to 25% of patients survive long term. The vast majority of patients do not survive and researchers do not fully understand why. A newer drug from Merck & Co., called Keytruda, acts on a different checkpoint called PD-1. (Keytruda knocked former President Jimmy Carter's metastatic melanoma into remission in 2015.) Recent trials that blocked both CTLA-4 and PD-1 improve long term survival to 60% of melanoma patients. Doctors are now combining checkpoint therapies with precision cancer drugs, and/or radiation, and/or chemotherapy. Checkpoint inhibitor therapy now helps extremely sick people live for years, not just months. Every cancer patient that is added to the success group is essentially cured. Top
Bristol-Myers Follows Breakthrough Yervoy With Opdivo

Opdivo (nivolumab), developed by the division of Bristol-Myers (Medarex) that developed Yervoy, limits the activity of checkpoint inhibitor PD-1 (similar to Keytruda). Opdivo has been approved by the US Food and Drug Administration (FDA) to treat melanoma, lung cancer, kidney cancer, blood cancer, head and neck cancer, and bladder cancer. Opdivo can cause side effects that may cause symptoms in many different parts of the body. Some side effects may need to be treated with other medicine, and some cancer treatments may be delayed.
-
Opdivo is used to treat metastatic melanoma, skin cancer that has metastasized (spread) that cannot be treated with surgery.
-
Opdivo is used to treat a certain type of non-small cell lung cancer. Opdivo may increase the chances for a longer survival time in people with this type of lung cancer.
-
Opdivo is used to treat advanced kidney cancer that has not responded to other cancer medicines, including Hodgkin's lymphoma that has relapsed after a stem cell transplant.
Opdivo is used to treat advanced squamous cell carcinoma of the head and neck that has progressed after a platinum-based therapy.
-
Opdivo is given alone or in combination with other cancer medicines. It is sometimes given after other medicines and proceedures have been tried without success.
Opdivo worked so well in its lung cancer trial that Bristol-Myers announced that it stopped the trial two years ahead of schedule. Lung cancer kills more Americans than any other type of cancer, about 160,000 a year. The Opdivo trial looked at a type of lung cancer called squamous cell non-small cell lung cancer, which accounts for about 20% to 30% of lung cancers. There have been "no other recent treatment breakthroughs" in squamous lung cancer, which commonly occurs in smokers or former smokers. So, the Opdivo advance was particularly welcome.
Existing cancer treatments - chemotherapy, radiation, surgery and targeted therapies – can help beat back tumors, but once the cancer has spread from its initial location, it is almost always a major issue. Immune therapy drugs offer the possibility that the immune system will keep a cancer in-check indefinitely.